
■ Physician-patient:
Disclosure of patient safety incidents

Introduction
When the clinical outcome is not as anticipated, physicians have an ethical, professional, and legal obligation to disclose harm from healthcare delivery to patients.
Despite a physician's dedication and commitment to provide the best care possible, an unanticipated outcome may arise. The Canadian Medical Association’s Code of Ethics and Professionalism states physicians must “take all reasonable steps to prevent or minimize harm to the patient; disclose to the patient if there is a risk of harm or if harm has occurred.” 1 In Québec, the Code of ethics of physicians states the doctor must “inform his patient or the latter’s representative of any incident, accident, or complication which is likely to have or has had a significant impact on his state of health or personal integrity.” 2
Some jurisdictions have also enacted legislation regulating the disclosure of patient safety incidents. Although different terms may be used, the intent of the legislation is to promote disclosure. Physicians should also be familiar with and follow any relevant guidelines or standards regarding disclosure set out by their medical regulatory authority (College) 3and any policies in place at the institution in which they practise.
The CMPA encourages frank, open discussions with patients after patient safety incidents. Nevertheless, after a legal action or College complaint has commenced, physicians should not continue to communicate with the patient directly. Physicians should consult with the CMPA as soon as possible in these circumstances.
The disclosure discussion:
- provides information
- promotes safe and quality medical care
- contributes to the maintenance of trust
- strengthens the physician-patient relationship
Maintaining trust with a patient having suffered a patient safety incident (accident in Québec) is rooted in having a strong pre-established physician-patient relationship. Establishing strong therapeutic relationships can be supported by:
- holding meaningful consent discussions
- exploring and setting realistic expectations for outcomes
- taking the time to understand and account for patient fears, ideas, feelings, and expectations
- taking the time to answer questions and explain concepts
Disclosure seeks to preserve the physician-patient relationship and to improve the quality and safety of healthcare. While disclosure may be stressful for patients, families and providers alike, it begins the emotional healing process and, where appropriate, the quality improvement investigation that seeks to prevent recurrences.
Good Practices
The World Health Organization (WHO) provides terminology to facilitate the sharing and learning of patient safety information globally. 4
Patient safety incident: An event or circumstance that could have resulted or did result in unnecessary harm to the patient.
Harmful incident: A patient safety incident that resulted in harm to the patient. This includes harm from system failures and performance issues of an individual provider.
No harm incident: A patient safety incident that reached the patient but no discernable harm resulted.
Near miss: A patient safety incident that did not reach the patient.
In Québec: The terms “accident and incident” are defined in the applicable legislation. Neither term corresponds exactly to the WHO terminology. An “accident” in Québec is defined as “an action or situation where a risk event occurs which has or could have consequences for the state of health or welfare of the user, a personnel member, an involved professional or a third person". The tem “incident,” on the other hand, is defined as “an action or situation that does not have consequences for the state of health or welfare of a user, a personnel member, an involved professional or a third person, the outcome which is unusual and could have had consequences under different circumstances.”
Following harm from healthcare delivery, patients have clinical, emotional, and information needs. Following an unexpected clinical outcome patients will want:
- an acknowledgement that something has gone wrong
- the facts that are known about what happened
- an understanding of the recommended next steps in clinical care
- a genuine expression of concern and regret
- reassurance that appropriate steps, if possible, are being taken to prevent a similar occurrence from happening again to themselves and to others
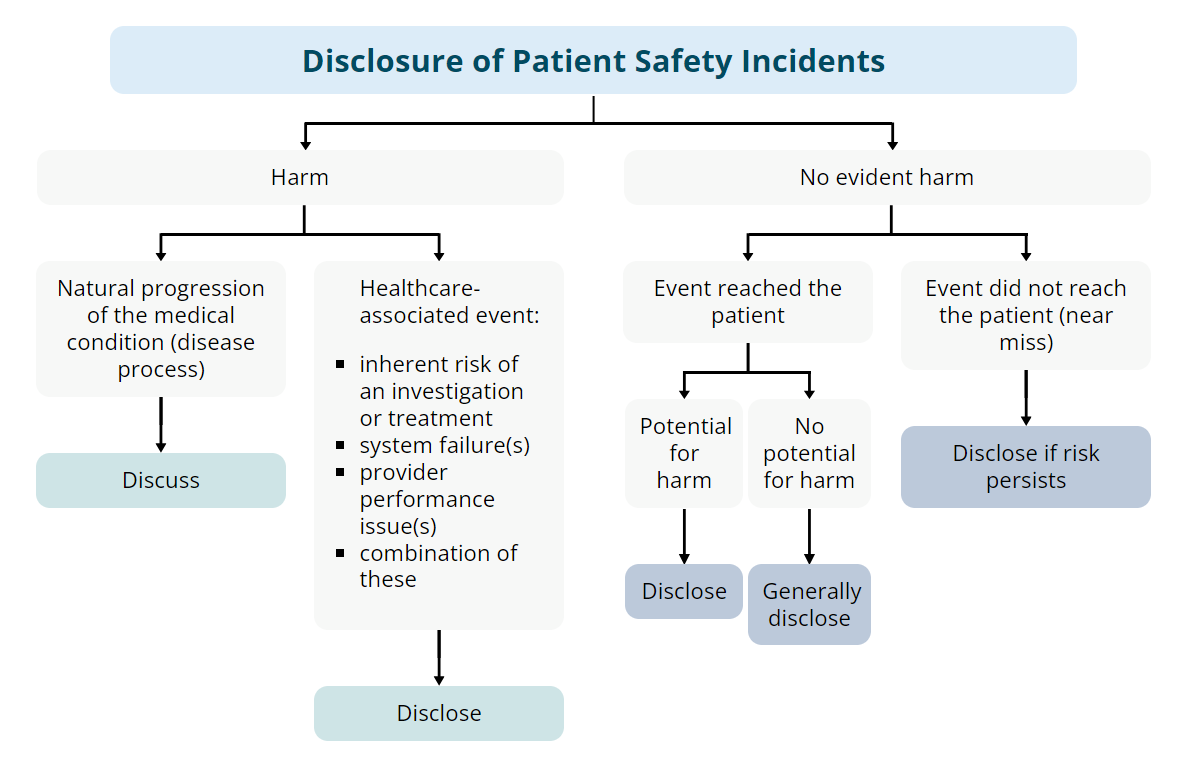
When unanticipated events occur, they may not necessarily result in harm to the patient. They may also be due to a number of circumstances, as outlined in the diagram below. Regardless of the nature of the event, it is generally advisable to be open and forthright about the facts with patients.
Disclosure of Patient Safety Incidents
-
Harm
-
Natural progression of the medical condition (disease process)
-
Discuss
-
-
- Healthcare-associated event:
- inherent risk of an investigation or treatment
- system failure(s)
- provider performance issue(s)
- combination of these
-
Disclose
-
-
No evident harm
-
Event reached the patient
-
Potential for harm
-
Disclose
-
-
No potential for harm
-
Generally disclose
-
-
-
Event did not reach the patient (near miss)
-
Disclose if risk persists
-
-
The Act to make the health and social services system more effective in Québec defines the terms accident and incident, and clarifies the need for disclosure of such events to patients. 5
The Code of Ethics of Physicians in Québec states that "A physician must, as soon as possible, inform his patient or the latter's legal representative of an accident or complication which is likely to have or which has had a significant impact on his state of health or personal integrity." 2
Disclosure of patient safety incidents in Québec
-
Harm
-
Natural progression of the medical condition (disease process)
-
Discuss
-
-
- Accident:
- inherent risk of an investigation or treatment
- system failure(s)
- provider performance issue(s)
- combination of these
-
Disclose
-
-
No evident harm
-
Incident
-
Event reached the patient
-
Potential for harm
-
Disclose
-
-
No potential for harm
-
Generally disclose
-
-
-
Event did not reach the patient (near miss)
-
Disclose if risk persists
-
-
-
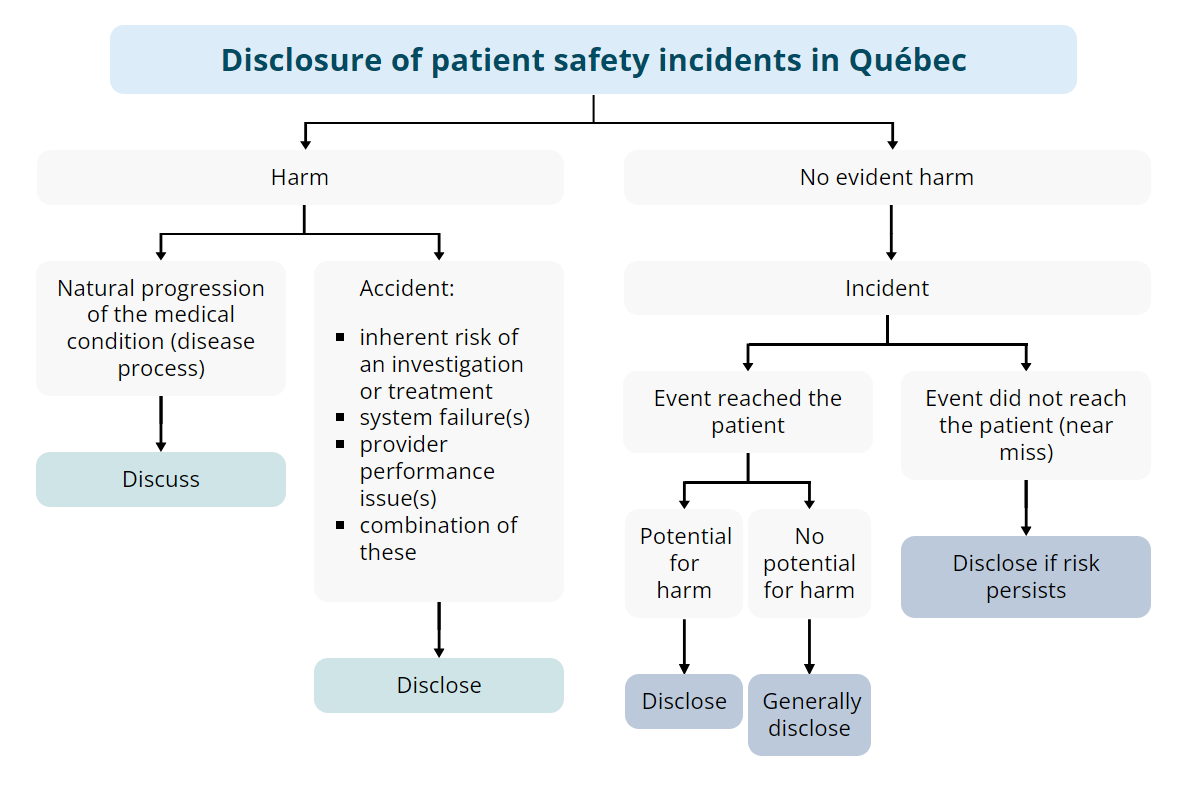
Accident
An accident is an action or situation where a risk event occurs that has or could have consequences for the state of health or welfare of the user, a personnel member, a professional involved, or a third person.
Any accident should be disclosed to the patient.
Incident
An incident is an action or situation that does not have consequences for the state of health or the welfare of the user, a personnel member, a professional involved or a third person, but the outcome of which is unusual and could have had consequences under different circumstances.
An incident, as the term is defined in Québec, may require disclosure if:
- the incident reached the patient but there were no consequences. Generally such incidents should be disclosed to patients.
- the incident did not reach the patient (i.e. the incident was caught in time) but the potential for harm existed. The patient should be informed of the incident if there is a similar, ongoing safety risk for that patient, or if the patient is aware of the incident and an explanation could allay concern and promote trust.
In Québec government-run institutions such as hospitals, the law requires the completion of a report in the prescribed format (form AH223), for both accidents and incidents. A copy of the report is kept with the patient's medical record. Completion of this form does not constitute disclosure to the patient. Rather, it serves to inform the institution’s administration of the event. As such, even when an event does not reach the patient, it is advisable to alert the patient to the incident, the report, and any subsequent preventive measures put in place. This will reduce the likelihood of misunderstanding or mistrust if the patient views the medical record and report in the future.
Sometimes unexpected events in healthcare delivery result in no evident harm. This can occur in the following situations:
No-harm incidents
The event reached the patient, but no harm occurred at the time and no potential for harm realistically exists in the future. However, sometimes an incident has the potential for harm, that is, harm might manifest in the future. For example, a patient exposed to poorly sterilized equipment might subsequently develop a viral infection. The infection would take time to declare itself and serial monitoring would be required. No-harm incidents require disclosure.
Near misses
The event did not reach the patient because of timely intervention or good fortune. In general, a near miss does not need to be disclosed, although there are exceptions. The patient should be informed about a near miss if there is a similar, ongoing safety risk for that patient, or if the patient is aware of the near miss and an explanation will allay concern and promote trust. If a near miss is documented in the medical record (such as in Québec through the use of an AH223 form), it is advisable to inform the patient of the near miss.
Disclosure is a process that may best unfold through discussions at each of two stages:
1. initial disclosure
The initial disclosure should:
- occur as soon as reasonably possible after the patient safety incident
- focus on the known facts, without speculation, and with special attention to the emotional and information needs of the patient
- convey empathy
- establish the way forward
Information should be provided regarding the investigative process that will be followed and what the patient can expect to learn. If known, specific timelines should be shared.
2. post-analysis disclosure
Some events may be reviewed by a quality improvement committee (medical, dental and pharmaceutical evaluation committee, in Québec) in your institution. Such reviews are undertaken to understand what factors contributed to the patient safety incident in order to help build better systems to avoid a reoccurrence.
Post-analysis disclosure
- focuses on the reasons for harm as determined by a post-event analysis
- provides a summary of any changes implemented to processes to decrease the likelihood of recurrence
- may involve an apology from the provider or institution, as appropriate
Throughout the disclosure process, patients benefit from knowing whom to contact if they have further concerns or questions. A designated staff person, such as a healthcare provider or administrator, can ensure the disclosure process advances properly and that the needs of the patient and providers are addressed.
1. First things first: Attend to clinical care
- Address clinical needs and deal with emergencies
- Consider the next steps in clinical care
- Obtain informed consent for any further required care
- Provide emotional support
- Document the patient safety incident
2. Plan the initial disclosure
- What are the facts?
- Who will be involved?
- When and where will the meeting occur?
- Seek help as appropriate
3. The initial disclosure meeting
- Provide the known facts
- Be sensitive
- Do not speculate or blame others
Consider the next steps in clinical care
Consider whether you are the appropriate individual or team to provide further care.
You should consider transferring the care of the patient in the event of any of the following:
- the patient requests or prefers it
- the patient's condition requires care you cannot provide
- you feel your emotional state may interfere with the provision of care now required.
Discuss the reasons for a transfer of care with the patient so they do not feel abandoned.
Determine the facts
The physician should communicate with the patient as soon as reasonably possible after the patient safety incident, focusing on the known facts and being prepared to provide further facts later as they become known. Before meeting with the patient, the most responsible physician (MRP) should determine the facts as known, to gain a preliminary understanding of what happened. This will likely include speaking to other healthcare providers involved in the patient safety incident and reviewing the medical record.
The reasons contributing to what happened will usually not all be known at the time of the initial disclosure and this will need to be explained to the patient.
The physician should organize his or her thoughts and reasoning prior to meeting with the patient, and prepare for emotional reactions and questions.
If possible, the physician should also confirm whether a quality improvement review concerning the patient safety incident will be conducted.
Determine who will be involved
Because they likely have the strongest relationship with the patient, the MRP should generally lead the meeting. If the MRP is not available, an appropriate delegate can lead the discussion and sensitively explain the reasons why the MRP is not available. Whoever leads should be in a position to provide the necessary information to the patient and be able to answer any clinical questions the patient may have.
The physician should seek input from the patient about whom they would like present during the discussion. Depending on the nature of the event or the anticipated reaction of the patient, with the patient's permission the attending physician may also consider having others present, such as:
- family members
- other healthcare providers directly involved with the care or who may provide important input on future care
- medical trainees
- skilled communicators
- a healthcare translator (preferably not a family member)
- those required to meet any special needs of the patient (e.g. cultural, vision, hearing, spiritual needs)
Begin with an expression of sympathy and compassion for the circumstances.
- provide the known facts
- be sensitive
- do not speculate or blame others
- provide emotional support
- plan to meet as often as necessary to support the patient and address their clinical, emotional, and information needs
Provide the known facts
No disclosure discussion will be perfect. Despite planning for the discussion and anticipating the patient's needs, there is no script to follow. Provide the known facts in a language patients will understand. Be careful not to jump to conclusions before all the facts are known.
Be sensitive
Be sensitive to how much information you provide and what your patient is ready to hear. Allow the patient to absorb the information at a rate they can manage. Don’t be afraid of silence—it provides an opportunity to process information and reflect.
Invite the patient to provide their perspective on what has happened and to express their needs. Good communication often involves listening more than talking: patients need to feel they have been heard.
Remember to be genuine, sincere, and compassionate. The perception that a physician has been dismissive of a patient’s concerns is a common reason for dissatisfaction and further complaint.
Do not speculate or blame others
Self-serving, defensive statements accompanied by blame for others will only increase tensions and are not helpful.
Provide emotional support
Patients and families experience a range of emotions following a harmful patient safety incident. Surprise may turn into mistrust, frustration, and anger. It is important to meet the emotional needs of your patients. Let them know you will be there for them. The aim is to support healing and maintain or restore trust.
Stating that you are sorry for the circumstances is appropriate at every disclosure meeting. Most patients and families will appreciate expressions of genuine concern and regret by a caring physician and healthcare team.
- If harm is the result of the progression of the underlying medical condition:
An expression of concern and sympathy is sufficient and could be appreciated by your patient and the family.
- If harm is related to an inherent risk of an investigation or treatment:
An expression of regret should be provided, such as "I am sorry this happened to you." An acceptance of responsibility should not be provided. It may be helpful to refer back to the consent discussion during conversations about a risk that materialized.
- In cases of harm with a clear and undeniable element related to provider or institutional performance (i.e. operating on the wrong patient or on the wrong site, giving the wrong medication):
An early apology should be considered by the responsible provider and/or responsible organization’s representative. A statement such as “I am sorry the wrong kidney was removed,” or “I am sorry, we removed the wrong kidney,” can be helpful to promote trust and convey empathy, even when the factors contributing to the patient safety incident have not yet been established. This could be followed by a statement such as “We do not know how this could have happened but we will be undertaking an analysis to determine how to prevent this from ever happening again.”
- If harm is NOT clearly related to provider performance or system failure at the time of the initial disclosure:
An apology may not be warranted until the completion of a quality improvement review of the event however an expression of regret should be provided, such as "I am sorry this happened to you."
In addition, in the post-analysis disclosure meeting:
- If after a careful analysis, the harm is determined to be related to system failures or provider performance:
An apology should be considered by the responsible provider or responsible organization's respresentative. At this stage, it is appropriate to acknowledge responsibility for the harm and to apologize.
The use of words that express or imply legal responsibility, such as negligence or fault, or reference to failing to meet the standard of care, should be avoided and are not required for an appropriate apology. Such legal determinations are complex, and independent bodies such as the courts and medical regulatory authorities (Colleges) have the responsibility to make these determinations fairly.
Apology legislation
Most Canadian provinces and territories have apology legislation in place. Apology legislation promotes the early resolution of disputes by reducing concerns about the legal implications of an apology. The legislation generally distinguishes between apologies and admissions of fault; specifically, expressions of regret or apologies should not be construed as admissions of fault or liability in the legal context.
Even if no apology legislation exists, it is still important to apologize to begin the emotional healing process.
After an appropriate analysis has taken place, any conclusive factual reasons for harm should be discussed with the patient. These reasons may include:
- factors related to an underlying medical condition
- recognized and unavoidable risks inherent in an investigation or treatment
- system failures
- problems with provider performance
- a combination of any of these
When system failure or provider performance issues are identified, it may be appropriate for the institution or the involved provider to provide an apology. This gesture is an important component of the patient’s healing process.
Post-analysis disclosure in community practice
In office or clinic settings, the supervising physician or the physician managing the clinic is likely to lead this discussion.
Patients usually appreciate learning of any changes made within the practice to prevent recurrences of a patient safety incident (accident in Québec).
Post-analysis disclosure in hospital and institutional settings
The hospital or institution leaders (i.e. risk management department) are typically responsible for the post-analysis disclosure. They determine what information will be disclosed to the patient at this stage. Limitations may exist on what information can be shared with patients, due to provincial/territorial legislation, regulations, institutional/hospital by-laws and policies, and legal privilege.
If the patient and the providers so choose, the hospital or institution should still provide the physician and other providers involved in the event with an opportunity to participate in these discussions.
If a physician has concerns about the clinical care delivered by another provider, that physician should consider first whether they know enough about the facts and circumstances. Many delays in diagnosis result from the variable progression of pathophysiology and symptoms and signs, and atypical presentations of diseases. As such, it is possible that while it may currently appear otherwise, the care provided by another physician was actually reasonable at the time, in the context of the available information.
It is important not to speculate or lay blame. An uninformed or thoughtless comment is unprofessional and often forms the basis for dissatisfaction and complaint by a patient or family member. Physicians should focus on the needs of the patient as they now exist and be mindful that their comments may themselves be harmful to patients.
In the spirit of learning, consider constructively discussing what happened and how the case evolved with the other provider, and invite them to participate in the disclosure discussion. This is especially important in cases that involve diagnostic imaging, laboratory, or pathological interpretations. A department chief or clinical supervisor may be helpful in giving a valuable perspective or in resolving a dispute. If there is concern about the care of another provider or the outcome, the original healthcare provider may be best suited to discuss their care with the patient and may appreciate the opportunity to do so.
It is helpful to alert the original provider of your or the patient's concerns as well as to the information you have already shared with the patient. The discussion should be supportive and non-judgmental.
Questioning whether an event constitutes a patient safety incident
Medical trainees are on the front lines of healthcare delivery and frequently will be the first to recognize a patient safety incident (accident in Québec ) has occurred. They may feel vulnerable when they witness what they believe to be harm from healthcare delivery that has not been recognized or disclosed to the patient. In such circumstances, trainees should consider a constructive and respectful course of action, asking themselves the following questions:
- Do I have sufficient knowledge of the facts to conclude this was a patient safety incident (accident in Québec)?
- If I am uncertain about the care provided or the need to disclose:
- Should I respectfully explore the rationale for the decision, action, or inaction with my supervisor?
- Is it appropriate to discuss this with a trusted mentor, being careful to maintain the confidentiality of the patient and the provider?
- Should I escalate the matter to the program director or the undergraduate dean?
Creating a culture of psychological safety and encouraging respectful speaking up will help resolve these concerns. Supervisors' supportive communication and willingness to help will make trainees feel comfortable voicing any anxiety they have about a particular issue, and thus promote safe medical care.
Participating in disclosure discussions
Trainees may be in a position where they can disclose facts to patients who have been harmed. Although faculty should strive to involve trainees in this important part of learning, it is also important to remember that a fulsome disclosure conversation is best held with the most responsible physician and appropriate team members also in attendance.
Documentation of the patient safety incident
Document the following facts in the progress notes:
- the facts as they are known (without speculation)
- the clinical situation as it now exists
- the consent discussions, options, and decisions made by the patient or family regarding any future clinical investigations and treatments
- any care provided
- any consultations and the rationale for these
Correcting the medical record
Generally, medical records should not be altered upon being notified of a lawsuit or complaint. Following a patient safety incident, if relevant clinical information is incorrect or incomplete, an addendum can be made, provided is it clearly marked as a correction. If existing information in the medical record is incorrect or incomplete and could pose an ongoing patient safety risk, this information can be carefully rectified. It is important to do this in a transparent way that makes it clear when and why the information was amended and by whom.
- Correct or modify only your own entries and do so by ensuring the additional entry is clearly labelled as such
- When missing information or mistakes are discovered, you may make an additional entry in the record, clearly marking it as an addendum or correction.
- Be aware of the relevant legal and medical regulatory authority (College) requirements for making late entries.
Corrections to an electronic record should follow the same principles as with a paper record.
If you wish to review a patient’s medical record but are no longer part of the patient’s circle of care, you may not be allowed to review it due to privacy laws or regulations. Seek permission from the custodian of the medical record (e.g. the medical records department) before doing so, or contact the CMPA.
Documentation of the disclosure discussion
Include the following details concerning the disclosure meeting:
- date, time, and location of the meeting
- name and roles of those present
- facts presented in the discussion
- participants' reactions and responses
- agreed-upon next steps
- any plan for providing follow-up and further information to the patient and family, if appropriate
- name and details of the patient's contact person
The CMPA encourages physicians to disclose patient safety incidents to patients as soon as reasonably possible. This can help maintain trust and prevent complaints.
Nevertheless, sometimes a patient may threaten to initiate a legal action or to lodge a College or hospital complaint.
If a patient has initiated a legal action or if you believe a patient has made a substantive threat to do so, it may be in the best interests of the patient to transfer their care to another physician. Even when there is no legal action, but if the trust in the physician-patient relationship has been damaged, it may be best to transfer care.
When a legal action, College complaint, or threat of a legal action has occurred, all communication with the patient should be conducted through the legal counsel assigned by the CMPA.
Patient safety incidents are stressful for patients and families, as well as for physicians and other healthcare providers. In some circumstances, if the emotional distress is significant, it may be prudent to transfer the patient’s care to another physician.
At all times, it is important for physicians to look after their own emotional and physical health.
- Seek emotional support from colleagues, trusted friends, family, or your own physician.
- In the course of these discussions, do not discuss clinical details and continue to safeguard patient health information.
- Consider seeking support and resources from provincial physician health programs, and visit the CMPA’s “Physician support and wellness" section.
Checklist: Disclosure
Disclosure seeks to support the physician-patient relationship and to improve the quality and safety of healthcare
Have you:
- Made the immediate clinical environment safe (e.g. removed malfunctioning equipment)?
- Obtained informed consent for ongoing care?
- Considered if you are the best individual to provide further care?
- Facilitated further care, if required?
Have you:
- Considered contacting the CMPA for advice?
- Scheduled the initial meeting with the patient as soon as reasonably possible?
- Gathered the known facts to gain a preliminary understanding of what happened?
- Differentiated fact from conjecture for the reasons underlying the event?
- Determined if there will be a quality improvement review?
- Anticipated the patient’s questions and reaction?
- Considered the patient’s wishes for whom should be present?
- Invited those individuals who have a direct role in providing clinical care and/or emotional support to the patient?
- Planned when and where the meeting will occur?
Have you:
- Considered contacting the CMPA for advice?
- Arranged for the presence of the most responsible physician (MRP)?
- Arranged a private area to meet with the patient?
- Arranged to be free from interruptions (i.e. handed over your pager or phone)?
- Begun the discussion with an expression of sympathy and compassion for the circumstances?
- Provided the known facts?
- Avoided jargon?
- Avoided speculating or laying blame?
- Addressed the patient’s information and emotional needs?
- Invited the patient to provide their perspective on what has happened?
- Remained sensitive and empathic?
- Remained professional and taken care not to appear defensive?
- Briefly outlined the quality improvement (QI) process that will be followed and what the patient and family can expect to learn?
- Discussed the timelines, if known, for the QI process?
- Assessed the patient’s level of understanding and satisfaction?
- Asked if there is anything further that can be done to assist the patient at this time?
- Provided the patient with the name and telephone number of a person whom they can contact?
- Arranged follow-up meetings?
- Provided genuine expressions of caring and support?
Have you:
- Considered contacting the CMPA for advice?
- Stated that you are sorry for the circumstances or the condition of the patient?
- Provided an expression of concern and sympathy (if the harm is the result of the progression of the underlying medical condition)?
- Expressed regret (if the reasons for the harm are unclear or if the harm is related to an inherent risk of an investigation or treatment)?
- Apologized, if the harm is clearly related to a “wrong” (wrong drug, wrong dose, wrong surgery, wrong patient, etc.)?
Have you:
- Considered contacting the CMPA for advice?
- Reviewed any new clinical facts, including conclusive factual reasons for the harm that the patient is entitled to learn?
- Determined if there are limitations on what information can be shared with patients?
- Arranged to participate in these discussions with the hospital leaders or the clinic manager, if the patient consents?
- Determined whether an apology from you is advisable?
Have you dated and documented:
- The patient safety incident?
- Any amendments or addition to the medical record?
- Meeting dates and times?
- Who participated?
- Matters discussed?
- The patient’s reaction and responses?
- Questions asked and answers provided?
- Agreements upon next steps?
- Expressions of empathy provided?
Additional resources
- "Physician-Team: Psychological safety", CMPA Good practices
- "Physician-Team: Delegation and supervision of trainees", CMPA Good practices
- "Physician-patient: Documentation and record keeping", CMPA Good practices
References
-
Canadian Medical Association. CMA Code of Ethics and Professionalism, 2018. Available from: https://www.cma.ca/cma-code-ethics-and-professionalism
-
Collège des médecins du Québec. Code of ethics of physicians, 2015. Available from: http://www.cmq.org/publications-pdf/p-6-2015-01-07-en-code-de-deontologie-des-medecins.pdf
-
For example, College of Physicians & Surgeons of Alberta. Standards of Practice: Disclosure of Harm, 2010 Jan. Available from: http://www.cpsa.ca/standardspractice/disclosure-of-harm/
-
World Health Organization. The Conceptual Framework for the International Classification for Patient Safety, 2009 Jan. Available from: https://www.who.int/patientsafety/implementation/taxonomy/ICPS-report/en/
-
Québec, An Act to make the health and social services system more effective, SQ 2023, c 34
DISCLAIMER: This content is for general informational purposes and is not intended to provide specific professional medical or legal advice, nor to constitute a "standard of care" for Canadian healthcare professionals. Your use of CMPA learning resources is subject to the foregoing as well as CMPA's Terms of Use.


