6 minutes
Published: April 2025
At the end of 2023, CMPA membership included 1,916 cardiologists (Type of Work 70).
The graph below compares the 10-year trends of cardiologists’ medico-legal experiences with those of all CMPA members.
What are the relative risks of a medico-legal case for cardiologists?
- Cardiologists, College (n=544)
- Cardiologists, Legal (n=200)
- All CMPA, College (n=47,958)
- All CMPA, Legal (n=13,970)
Between 2014 and 2023, cardiologists consistently had significantly lower rates of College complaints 1 compared to all CMPA members (P<.0001).
The rates of civil legal actions for cardiologists were comparable to those of all CMPA members.
What are your risk levels regarding medico-legal cases, compared to other cardiologists?
Percentage of cardiologists, 5-year case frequency
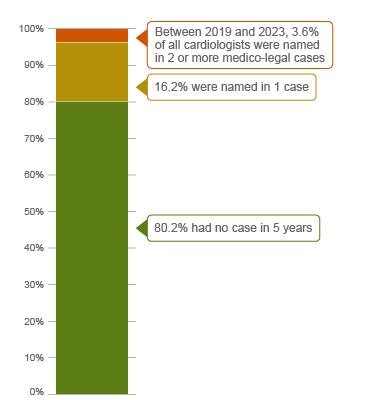
| No case |
80.2 |
| 1 case |
16.2 |
| 2 cases or more |
3.6 |
Percentage of cardiologists, 1-year case frequency
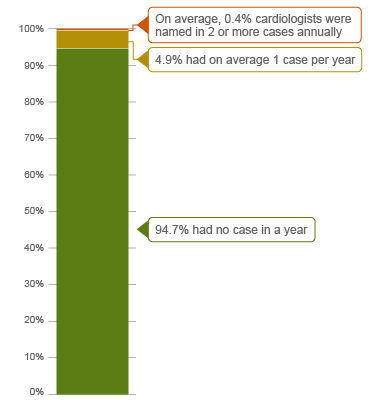
| No case |
94.7 |
| 1 case |
4.9 |
| 2 cases or more |
0.4 |
Approximately 80% of all cardiologists were not involved in any medico-legal case (including civil legal action, College or hospital complaint) over a 5-year period between 2019 and 2023 2. Under 4% were named in 2 or more new medico-legal cases.
Annually, 5% of cardiologists had on average one case per year, another 0.4% had two or more cases per year (the highest frequency of cases).
The following sections describe the findings based on the 454 cases with peer expert criticism, including civil legal actions, College, and hospital complaints involving cardiologists that were closed by the CMPA between 2014 and 2023.
What are the most common patient complaints and peer expert 3criticism? (n=454)
| Deficient assessment |
37 |
11 |
| Diagnostic error |
33 |
16 |
| Communication breakdown with patient/family |
25 |
12 |
| Inadequate monitoring or follow-up |
21 |
10 |
| Unprofessional manner |
18 |
4 |
| Failure to perform test or intervention |
18 |
10 |
| Inadequate consent process |
14 |
6 |
| Poor decision-making regarding management |
9 |
3 |
| Failure to refer |
8 |
4 |
| Injury associated with healthcare delivery |
8 |
8 |
Complaints are reflective of the patient’s perception that an issue occurred during care. These complaints are not always supported by peer expert opinion. Peer experts may not be critical of the care provided, or may have criticisms that are not part of the patients’ allegation.
The most frequent peer expert criticisms are:
- Communication breakdown with patient or family. For example, failure to: inform the patient of potential side-effects of medication; return patient phone calls in a timely manner; inform patient of the obligation and intent to report to the provincial/territorial motor vehicle licensing authority in the event that the patient may be unfit to drive or may lead to driver’s license suspension; describe the nature of cardiac exam before proceeding.
- Deficient assessment. For example, failure to: review prior investigations such as past ECGs; adequately investigate a patient with chest pain; consider patient’s medical history; examine patient with signs of stroke after an angiogram.
- Failure to perform test/intervention. For example, delay or failure to order diagnostic testing such as echocardiogram, CT to rule out aortic dissection, or Holter monitor.
- Inadequate monitoring or follow-up. For example, failure to: monitor a patient on long term amiodarone therapy for toxicity; order continuous cardiac monitoring. Follow up on investigations such as a stress test.
- Inadequate documentation. For example, failure to document: medical history, physical exam, complications that occurred during a procedure, changes seen on ECG, consent discussion, and/or clinic visits.
What are the most frequent presenting conditions in medico-legal cases involving cardiologists? (n=454)
- Ischemic heart disease (e.g. atherosclerotic heart disease, myocardial infarction, angina) (95)
- Arrhythmias (e.g. atrial fibrillation, heart blocks) (70)
- Valve disorders (e.g. aortic and/or mitral valve stenosis or insufficiency) (36)
- Heart failure (e.g. congestive heart failure) (30)
- Congenital malformations of the circulatory system (e.g. atrial septal defect, coarctation of the aorta) (26)
- Cardiomyopathies (17)
Out of the 454 cases, 72 patients experienced a missed diagnosis, a delayed diagnosis or a misdiagnosis. Peer expert criticism related to diagnostic cases included:
- Failure to diagnose a thromboembolic event post-angiogram
- Delay in performing an echocardiogram, leading to a delay in diagnosis of a myxoma
- Misdiagnosing a patient with pulmonary hypertension after misinterpreting an echocardiogram
The most frequent invasive procedures performed by cardiologists included cardiac catheterization, cardiac angiography, ablation, and pacemaker insertion.
Frequencies of presenting conditions and treatment procedures among medico-legal cases are likely representative of cardiologists’ practice patterns and do not necessarily reflect high-risk areas.
What are the top factors associated with severe patient harm 4 in medico-legal cases? (n=454)

Patient factors 5
- Aged 65 or over
- Obesity
- Presenting with or history of
- Ischemic heart disease, e.g. myocardial infarction, angina, atherosclerotic heart disease
- Renal failure
- Diseases of arteries, arterioles and capillaries, e.g. aortic dissection/aneurysms, peripheral vascular disease, arterial atherosclerosis
- History of episodic and paroxysmal disorder (e.g. sleep apnea, TIA)
- Having complication of
- Injuries to the thorax, e.g. heart puncture/laceration
- Cerebrovascular diseases, e.g. cerebral infarction
- Other disorders of the nervous system, e.g. anoxic brain injury
- Ischemic heart disease, e.g. myocardial infarction, atherosclerotic heart disease, angina
- Undergoing an invasive surgical procedure performed by a cardiologist or other specialists
Provider factors 6
- Failure to perform test/intervention, e.g. Holter monitor, diagnostic imaging such as CT scan or angiogram
- Failure to refer
- Inappropriate transfer
- Failure to transfer
- Inadequate monitoring or follow-up
Team factors 6
- Inadequate communication with other physicians
- Inadequate documentation
Risk reduction reminders
In an in-depth review of medico-legal cases, the following risk management considerations have been identified for cardiologists based on peer expert criticisms:
- Gather an appropriate history, including comorbidities and current medications, and conduct an appropriate systematic physical examination with vital signs. Include a review of current status and investigations.
- Consider which diagnostic tests or consultations are necessary to establish or confirm the diagnosis. Review investigative findings to ensure they correspond with the clinical impression and arrange appropriate follow-up to investigate any discrepancy.
- Ensure there is a reliable system in place to facilitate the timely receipt, review, and appropriate management and follow-up of investigative tests, including communicating results to patients. Periodically evaluate and engage in quality improvement of that system to address any quality gap.
- Document in the medical record the patient’s history (including symptoms and comorbidities), physical exam findings, reassessments, differential diagnoses, investigations, diagnosis, and reasoning. Include any treatment plan and follow-up instructions you have shared with the patient, their caregiver, or family.
- Demonstrate empathy and support. Ensure that the patient’s (and family’s) questions and concerns are acknowledged and addressed. Utilize active listening techniques and tailor the communication to meet the diverse needs of patients and their families.
Limitations
The numbers provided in this report are based on CMPA medico-legal data. CMPA medico-legal cases represent a small portion of patient safety incidents. Many factors influence a person’s decision to pursue a case or file a complaint, and these factors vary greatly by context. Thus, while medico-legal cases can be a rich source for important themes, they cannot be considered representative of patient safety incidents overall.
Now that you know your risk…
Mitigate your medico-legal risk with CMPA Learning resources.
- CMPA Research:
- CMPA Learning:
Looking for more?
For any data request, please contact [email protected]
Notes
-
Physicians voluntarily report College matters to the CMPA. Therefore, these cases do not represent a complete picture of all such cases in Canada.
-
It takes an average of 2-3 years for a patient safety incident to progress into a medico-legal case. As a result, newly opened cases may reflect incidents that occurred in previous years.
-
Peer experts refer to physicians who interpret and provide their opinion on clinical, scientific, or technical issues surrounding the care provided. They are typically of similar training and experience as the physicians whose care they are reviewing.
-
Severe patient harm includes death, catastrophic injuries and major disabilities. Healthcare-related harm could arise from risk associated with an investigation, medication or treatment. It could also result from failure in the process of patient care.
-
Patient factors include any characteristics or medical conditions that apply to the patient at the time of the medical encounter, or any events that occur during the medical encounter.
-
Based on peer expert opinions. These include factors at provider, team, and system levels. For cases involving cardiologists, there is no evidence for system level factors in the data.