5 minutes
Published: January 2025
At the end of 2023, 773 CMPA members were dermatologists (Type of Work 44).
The graph below compares the 10-year trends of dermatologists’ medico-legal experiences with those of all CMPA members.
What are the relative risks of a medico-legal case for dermatologists?
- Dermatologists, College (n=672)
- Dermatologists, Legal (n=156)
- All CMPA, College (n=47,958)
- All CMPA, Legal (n=13,970)
Between 2014 and 2023, dermatologists consistently had significantly higher rates of College complaints 1 than all CMPA members (p<0.0001).
Compared to all CMPA members, the overall rate of civil legal actions for dermatologists was also significantly higher (p <0.0001).
How does your medico-legal risk exposure compare to other dermatologists?
Percentage of dermatologists, 5-year case frequency
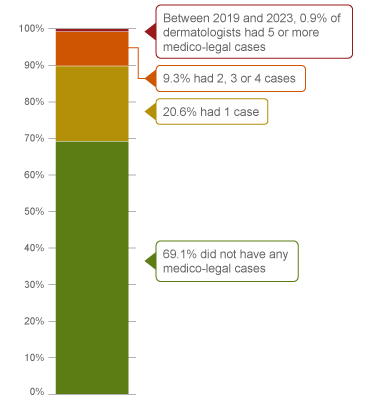
| No case |
69.1 |
| 1 case |
20.6 |
| 2-4 cases |
9.3 |
| 5 cases or more |
0.9 |
Percentage of dermatologists, 1-year case frequency
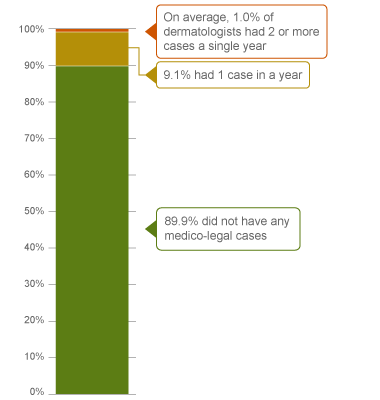
| No case |
89.9 |
| 1 case |
9.1 |
| 2 cases or more |
1.0 |
|
In a 5-year period (2019 – 2023) 2, 31% of all dermatologists were named in a medico-legal case. 9% were named in 2, 3 or 4 cases. These dermatologists had more cases than 90% of other dermatologists who had either 0 or 1 case in five years. Under 1% of dermatologists had 5 or more cases in this 5-year period (the highest frequency of cases).
Annually, 1% of dermatologists had an average of 2 or more cases in a year, and therefore had more cases than 99% of other dermatologists.
The following sections describe the findings based on the 433 civil legal cases, College, and hospital complaints involving dermatologists that were closed by the CMPA between 2014 and 2023.
What are the most common patient complaints and peer expert 3 criticisms? (n=433)
| Deficient assessment |
35 |
11 |
| Diagnostic error |
27 |
16 |
| Unprofessional manner |
24 |
8 |
| Communication breakdown with the patient or family |
19 |
22 |
| Inadequate office procedure |
16 |
17 |
| Inadequate consent process |
16 |
12 |
| Failure to perform test or intervention |
12 |
18 |
| Inadequate monitoring or follow-up |
11 |
7 |
| Professional misconduct |
8 |
6 |
| Injury associated with healthcare delivery |
8 |
3 |
Complaints are driven by the perception that a problem or medical issue occurred during care. These complaints are not always supported by peer expert opinion. Peer experts may not be critical of the care provided, or may have criticisms that are not part of the patients’ allegation.
In these 433 cases, peer experts often criticized the dermatologist’s communication with patient or family, and the administrative or organizational management of their office.
What are the most frequent conditions associated with dermatologists’ care? (n=433)
- Melanoma and other malignant neoplasms of skin (81)
- Infectious diseases (44)
- Radiation-related disorders of the skin and subcutaneous tissue (e.g. actinic keratosis) (39)
- Other skin conditions (e.g. acne, rosacea, psoriasis) (36)
- Epidermal conditions (e.g. seborrheic keratosis) (33)
Frequencies of presenting conditions among medico-legal cases are likely representative of dermatologists’ practice patterns and do not necessarily reflect high-risk conditions.
Out of the 433 cases, 69 patients experienced a missed diagnosis, a delayed diagnosis or a misdiagnosis. Peer expert criticism related to diagnostic cases included:
- Failure to perform test or intervention, such as biopsy or lesion removal. For example, a patient with a history of sun damage was diagnosed with seborrheic keratosis and treated with electrodessication without performing a biopsy. The patient was later diagnosed with melanoma resulting in multiple progressive metastases and the patient’s death.
- Deficient assessment, such as failing to perform a focused clinical assessment including a complete medical and family history, a review of previous test results, and an examination of lesions. For example, when a patient was referred for lesions on the head and neck, a dermatologist failed to offer a full dermatological survey for malignancy, and failed to document this discussion with the patient.
- Inadequate documentation that lacks details such as: the appearance, size, symmetry, border regularity or lack thereof, texture or consistency of the lesion; a differential diagnosis and reasoning for treatment choice; treatment plan; consent discussion; and follow-up plan. For example, a dermatologist’s notes lacked the necessary details for another physician to be able to review the patient’s care. There was no evidence in the chart that the dermatologist had provided the patient with a prescription, discussed follow-up or sent a consultation letter to the referring physician.
- Inadequate monitoring or follow-up such as disclosing test results to the patient, and ensuring appropriate follow-up of care. For example, a dermatologist’s failure to follow up on the biopsy results in a timely manner resulted in a delay in the patient’s cancer diagnosis and treatment.
- Communication breakdown with the patient and/or their family. For example, failing to clearly discuss the diagnosis severity, treatment options, need for referral, steps of the procedure and discharge instructions.
What are the top factors associated with patient harm 4 in medico-legal cases? (n=433)

Patient factors 5
- Presenting with or progression of melanoma and other malignant neoplasms of the skin
- Complications of treatments:
- Scarring
- Infection
- Deformity
- Acute pain
Provider factors 6
- Failure to perform test/intervention (e.g. biopsy)
- Inadequate monitoring or follow-up (e.g. failure to notify the patient of the pathology results)
- Improper operation or misuse of equipment (e.g. inappropriate laser settings causing burns)
Risk reduction reminders
The following risk management considerations have been identified for dermatologists.
- Ensure that investigations are appropriately scheduled and performed, and that the resulting report is received and followed up in a timely manner. Discuss pertinent negative or reassuring findings with the patient, and document the discussion. When communicating the test results to patients, avoid using the "no news is good news" approach.
- Tailor your communication to meet the diverse needs of patients and their families while utilizing active listening techniques for clear and effective communication. Ensure that the patient's and family's questions and concerns are acknowledged and addressed.
- Obtain a detailed patient history, determine the appropriate procedure or medication that aligns with the patient's health goals, and discuss reasonable alternative options. Carefully consider the indications for the procedure or medication, especially in high-risk patients.
- In obtaining informed consent, physicians should discuss and document the diagnosis, proposed treatment, chances of success or anticipated results, treatment options (including non-treatment and its potential consequences), and material and special risks associated with the proposed and alternative treatments (including rare but important risks of major consequences). In the same discussion, ensure the patient's understanding and expectations, and answer any questions.
- The supervising physician should ensure that non-physician providers have the required knowledge, skills, and experience to perform the task. The supervising physician should determine the degree of required supervision and ensure the patient has been notified of the non-physician provider’s qualifications.
Limitations
The numbers provided in this report are based on CMPA medico-legal data. CMPA medico-legal cases represent a small portion of patient safety incidents. Many factors influence a person’s decision to pursue a case or file a complaint, and these factors vary greatly by context. Thus, while medico-legal cases can be a rich source for important themes, they cannot be considered representative of patient safety incidents overall.
Now that you know your risk…
Mitigate your medico-legal risk with CMPA resources.
- CMPA Research:
- CMPA Learning:
Looking for more?
For any data request, please contact [email protected]
This report received input and review from Dr. Susan Swiggum. We appreciate Dr. Swiggum’s contribution to CMPA research work.
Notes
-
Physicians voluntarily report College matters to the CMPA. Therefore, these cases do not represent a complete picture of all such cases in Canada.
-
It takes an average of 2-3 years for a patient safety incident to progress into a medico-legal case. As a result, newly opened cases may reflect incidents that occurred in previous years.
-
Peer experts refer to physicians who interpret and provide their opinion on clinical, scientific, or technical issues surrounding the care provided. They are typically of similar training and experience as the physicians whose care they are reviewing.
-
Includes moderate, severe patient harm and death. In the CMPA Research glossary, moderate patient harm is defined as symptomatic, requiring intervention or an increased length of stay, or causing permanent or temporary harm, or loss of function. Severe patient harm is defined as symptomatic, requiring life-saving intervention or major medical/surgical intervention, or resulting in a shortened life expectancy, or causing major permanent or temporary harm or loss of function.
-
Patient factors include any characteristics or medical conditions that apply to the patient at the time of the medical encounter, or any events that occur during the medical encounter.
-
Based on peer expert opinions.