At the end of 2023, 680 CMPA members were plastic surgeons (Type of Work 86).
The graph below compares the 10-year trends of plastic surgeons’ medico-legal experiences with those of all surgical specialties.
What are the relative risks of a medico-legal case for plastic surgeons?
- Plastic surgeons, College(n=727)
- Plastic surgeons, Legal(n=713)
- All surgical specialists, College(n=7,307)
- All surgical specialists, Legal(n=4,448)
Between 2014 and 2023, the overall rate of College matters 1 for plastic surgeons was significantly higher than the rate of all surgical specialties (p<.0001).
Compared to all surgical specialties, plastic surgeons consistently had significantly higher rates of civil legal actions (p<.0001).
What are your risk levels regarding medico-legal cases, compared to other plastic surgeons?
Percentage of plastic surgeons, 5-year case frequency

| No case |
50.6 |
| 1 case |
26.1 |
| 2-4 cases |
18 |
| 5 cases or more |
5.3 |
Percentage of plastic surgeons, 1-year case frequency
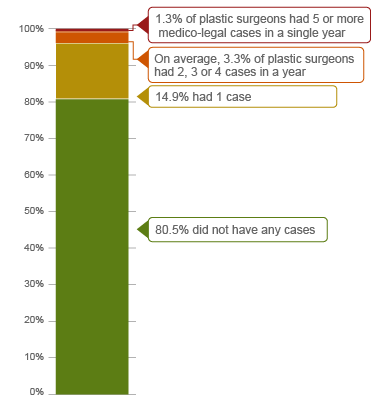
| No case |
80.5 |
| 1 case |
14.9 |
| 2 cases or more |
4.4 |
| 5 cases or more |
0 |
In the recent 5 years (2019 – 2023) 2, 18% of all plastic surgeons were named in 2, 3, or 4 cases (including legal actions, College or hospital complaints). This means they had more cases than 76.7% of other plastic surgeons who had 0 or 1 case. In the 5-year period, 5.3% of plastic surgeons had 5 or more cases.
On average, 4.4% of plastic surgeons had 2 or more cases annually. The annual case frequencies were higher than 95.4% of all plastic surgeons.
In the civil legal actions, College and hospital matters closed in CMPA in the past 10 years (2014 – 2023), we identified 987 cases with peer experts providing opinion on the care provided by a plastic surgeon. In 426 (43.2%) of these cases, plastic surgeons performed non-cosmetic 3 procedures. The following sections focus on findings from the 426 cases.
What are the most common patient complaints and peer expert 4 criticisms? (n=426)
| Deficient assessment |
35 |
13 |
| Inadequate consent process |
24 |
11 |
| Diagnostic error |
22 |
14 |
| Failure to perform test or intervention |
20 |
10 |
| Inadequate monitoring or follow-up |
20 |
8 |
| Communication breakdown with the patient |
18 |
11 |
| Unprofessional manner |
17 |
4 |
| Injury associated with healthcare delivery |
12 |
6 |
| Poor decision-making regarding management |
12 |
5 |
| Insufficient knowledge or skill |
11 |
5 |
Complaints are a reflection of the patient’s perception that a problem occurred during care. These complaints are not always supported by peer expert opinion. Peer experts may not be critical of care provided or may have criticisms that are not part of the patients’ allegation.
What are the most frequent interventions with peer expert criticism? (n=426)
- Breast reconstruction following mastectomy (41)
- Release of nerve(s) of the forearm and wrist (e.g. carpal tunnel release) (26)
- Breast reduction (25)
- Transurethral resection of the prostate (TURP) (17)
- Release of soft tissue of wrist and hand (e.g. Dupuytren's contracture release) (15)
- Release of flexor tendons of finger (e.g. trigger finger release) (13)
Peer expert criticisms
- Inadequate documentation
- Inadequate consent process
- Deficient assessment
- Communication breakdown with patient
- Inadequate monitoring or follow-up
- Poor decision-making regarding management
Intervention frequencies among medico-legal cases are likely representative of plastic surgeons’ practice patterns and do not necessarily reflect high-risk interventions.
Of the 426 cases, 61 patients had diagnostic error. For example:
- The plastic surgeon failed to recognize that the patient's symptoms were signs of a nerve injury and failed to act accordingly.
- A plastic surgeon underestimated the severity of a patient’s burns and therefore failed to implement a burn protocol.
Twenty-three patients had injuries. For example:
- A patient developed complex regional pain syndrome after carpal tunnel release surgery when the plastic surgeon failed to provide adequate postoperative follow up.
In addition, 15 patients received the wrong procedure. For example:
- The plastic surgeon obtained punch biopsy sample from the wrong lesion when they failed to review the consult from the referring physician.
What are the top factors associated with severe patient harm 5 in medico-legal cases? (n=426)

Patient factors 6
- History of major surgery
- Current smoker
- Post-operative complications of
- Progression or metastases of cancer
- Breast disorder (e.g. breast asymmetry, necrosis of the nipple)
- Wound infection
- Injury during provision of healthcare (e.g. hematoma, wound dehiscence)
Provider factors 7
- Deficient assessment
- Inadequate monitoring or test result follow-up
- Failure to perform test or intervention (e.g. nerve conduction studies for patient with ongoing hand weakness after carpal tunnel release surgery)
- Poor clinical decision-making regarding patient management (e.g. failure to obtain and review all test results prior to performing skin biopsy; failure to appropriately manage patient with second-degree burns)
- Insufficient knowledge or skills (e.g. misdiagnosis of a squamous cell carcinoma; failure to ensure adequate margins of excised melanoma)
Risk reduction reminders
An in-depth review of medico-legal cases involving plastic surgeons performing non-cosmetic surgeries highlights the need for ongoing education related to the following areas.
Pre-operative
- Maintain an awareness of the patient’s co-morbidities and surgical history. Include a review of current status and investigations.
- Ensure all test results and pre-op imaging have been reviewed and are available in the patient’s chart for review on the day of surgery.
- When communicating the test results to patients, avoid using the "no news is good news" approach. Discuss pertinent negative or reassuring findings with the patient, and document the discussion.
Intra-operative
- Consider the risks of intra-operative injuries during all phases of surgical care. Take precautions to protect vital structures such as nerves and vasculature, and document any efforts to visualize or protect these structures. Consider altering technique or consulting a colleague when difficulties are encountered during surgery.
Post-operative
- Certain suboptimal outcomes reflect the inherent risks of a procedure; however, others can generally be avoided with appropriate planning and safety protocols. Ensure diligent follow-up of actual or potential complications to improve patient outcomes and reduce the risks of medico-legal difficulties.
- Discuss discharge instructions with patients, including signs/symptoms to monitor and guidance for when to seek medical attention; provide follow-up care as needed.
In general, keep up to date with clinical standards and meet requirements for continuing medical education and professional development.
Limitations
The numbers provided in this report are based on CMPA medico-legal data. CMPA medico-legal cases represent a small portion of patient safety incidents. Many factors influence a person’s decision to pursue a case or file a complaint, and these factors vary greatly by context. Thus, while medico-legal cases can be a rich source for important themes, they cannot be considered representative of patient safety incidents overall.
Now that you know your risk…
Mitigate your medico-legal risk with CMPA resources.
- CMPA Research:
- CMPA Workshops:
- CMPA eLearning:
Looking for more?
For any data request, please contact [email protected]
This report received input from Dr. Jugpal Arneja; we appreciate his contribution.
Notes
-
Physicians voluntarily report College matters to CMPA. Therefore, these cases do not represent a complete picture of all such cases in Canada.
-
It takes an average of 2-3 years for a patient safety incident to progress into a medico-legal case. As a result, newly opened cases may reflect incidents that occurred in previous years.
-
Non-cosmetic cases refer to non-aesthetic cases focused on reconstructing the form of the body after trauma or defect, and body enhancement procedures designed to correct or improve the body's function or overall health.
-
Peer experts refer to physicians who interpret and provide their opinion on clinical, scientific, or technical issues surrounding the care provided. They are typically of similar training and experience as the physicians whose care they are reviewing.
-
Includes moderate, severe patient harm, and death. In the CMPA Research glossary, moderate harm is defined as symptomatic, requiring intervention or an increased length of stay, or causing permanent or temporary harm, or permanent or temporary loss of function. Severe patient harm is defined as symptomatic, requiring life-saving intervention or major medical/surgical intervention, or resulting in a shortened life expectancy, or causing major permanent or temporary harm, or major permanent or temporary loss of function.
-
Patient factors include any characteristics or medical conditions that apply to the patient at the time of the medical encounter, or any events that occur during the medical encounter.
-
Based on peer expert opinions. These include factors at provider, team, and system levels. For non-cosmetic plastic surgeries, there is no evidence for team or system level factors in the data.