Harm related to healthcare may occur despite the dedication, training, and professionalism of healthcare providers. An important part of a "just culture of safety" is learning from patient safety incidents (accidents in Québec) and near misses”. Quality improvement is a key tool that can help build increasingly reliable processes and systems that promote safe care.
The following are commonly used terms and approaches for quality and safety improvement.
Good practice guidance
Patient safety incidents and near misses are most often approached in one of two ways, exist. The “name, blame and shame approach,” focuses on identifying the providers who had the last contact with the patient, singling them publicly out for their failure to prevent the incident, and calling for greater vigilance, better training, and sometimes administering professional sanctions. A more productive approach for encouraging continuous improvement, based on Reason’s Systems theory, emphasizes that focusing on the system rather than on the individual has the potential to prevent far more patient safety incidents. 3
The key to the successful application of the systems theory is to strike a balance in acknowledging both individual and system contributions in the genesis of an incident or near miss. In the just culture approach, organizational leaders and managers are accountable for designing reliable systems and managing the behaviour of employees/providers, while individual providers are accountable for the quality of their work including their behavioural choices, and for reporting concerns about potential safety issues. Within this framework, providers are held accountable for what is in the realm of their control—their behaviours—but not for systems issues over which they have no control.
The Swiss Cheese model
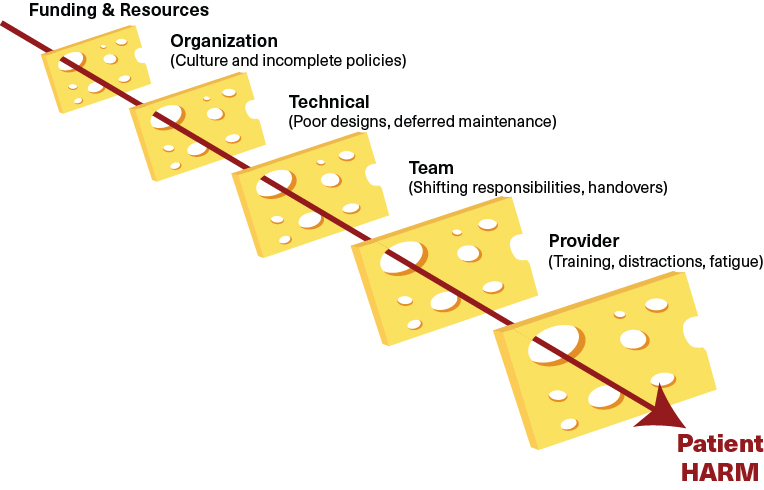
The visualization of the Swiss Cheese Model consists of five slices of Swiss Cheese, representing the defensive barriers or safeguards for patients. Examples given include funding and resources, organization, technical, team and provider barriers. The holes in each slice represent weaknesses or possible failure points in each part of the healthcare system:
- Funding & Resources
- Organization (Culture and Incomplete policies)
- Technical (Poor designs, deferred maintenance)
- Team (Shifting responsibilities, handovers)
- Provider (Training, distractions, fatigue)
Harm is depicted as an arrow that passes through aligned holes in different swiss cheese layers.
The Swiss Cheese model by Dr. James Reason illustrates how system failure may lead to harm
The defensive barriers or safeguards for patients may be thought of as slices of Swiss cheese. Usually the slices are protective. However, as systems are by nature imperfect, each slice has vulnerabilities. Each hole represents weaknesses or possible failure points, which may be continually opening, closing, or changing location, reflecting the dynamic nature of complex systems.
The system is safer by the redundant nature of protective barriers, where in this case it is unlikely that the holes in the cheese all line up to allow for harm (represented by several slices of cheese next to one another). Patient safety incidents in healthcare usually occur because of failures in successive layers of protection.
Safety is improved by minimizing the number and size of “holes” in our safety net, to reduce the likelihood that similar types of patient safety incidents will occur in the future. This means not only strengthening the system of knowledge and skills of providers, but also the system and processes of care in the workplace.
More and more, there is recognition that patients can be another effective layer of protection. When they are included as part of the healthcare team and have appropriate information, they can help decrease some of the inherent risks.
Collapse section
A safety culture is an everyday set of principles grounded in the protection of the values of healthcare delivery. The just culture model is a values-supportive system of shared accountability.
In a just culture of safety, outcomes are not prejudged, the interests of both patients and providers are protected, and the focus is on learning to prevent future incidents (as opposed to blaming). Patient safety incidents are analyzed to support and educate administrators, healthcare providers, and patients to prevent similar events in the future. The professional accountability of healthcare providers is determined fairly.
The Institute for Healthcare Improvement (IHI) and Safe & Reliable Healthcare offer a framework that can be helpful for leaders in planning and designing highly reliable healthcare delivery systems. 4
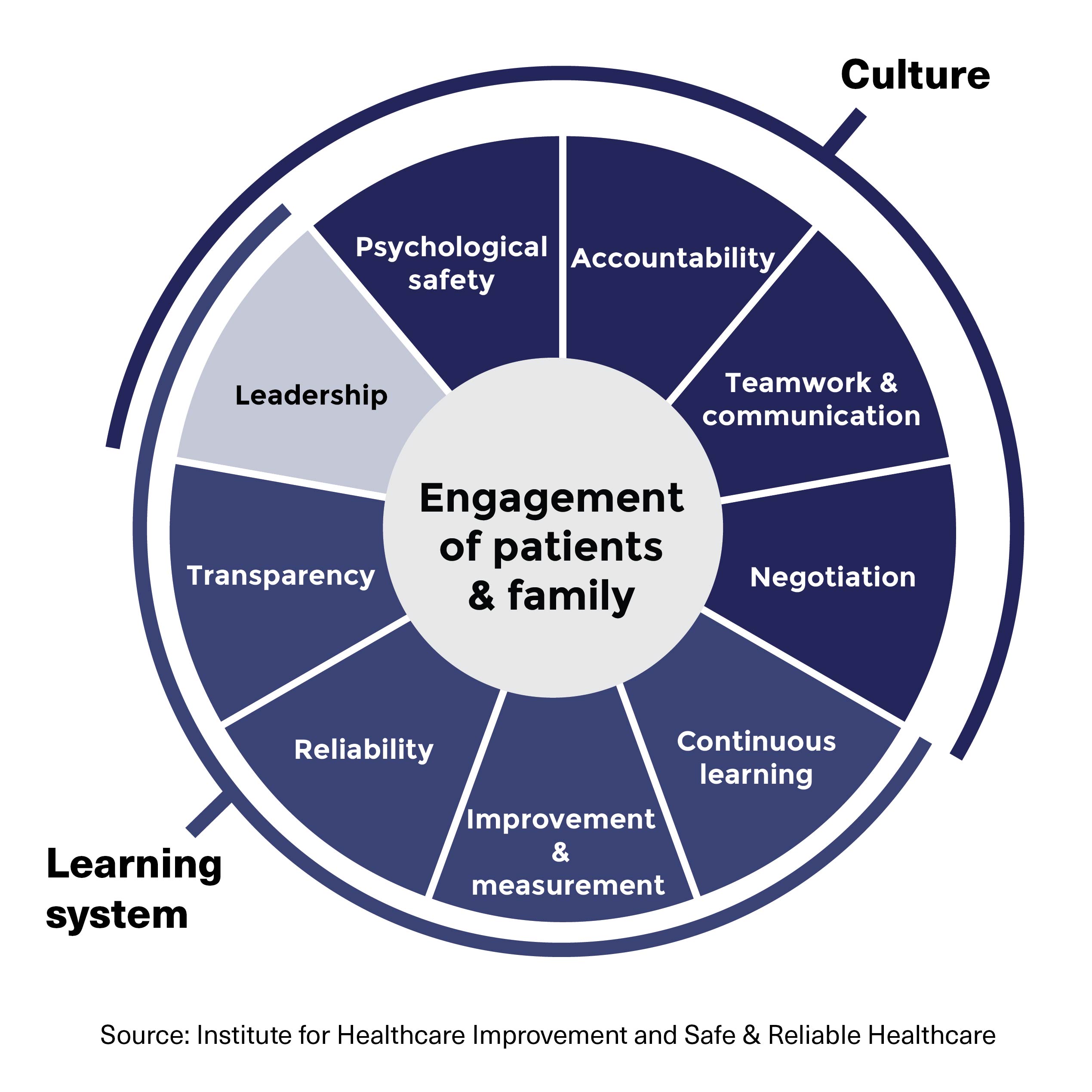
The Institute for Healthcare Improvement (IHI) and Safe, Reliable and Effective Healthcare framework depicts workplaces as a ring-shaped puzzle with a dark blue half representing culture and a medium blue half representing the learning system. The dark blue culture half is composed of four puzzle pieces: psychological safety, accountability, teamwork and communication and negotiation. The medium blue learning system half is composed of four puzzle pieces: transparency, reliability, improvement and measurement and continuous learning. Both sides of the ring are linked by a puzzle piece labelled leadership. The ring-like puzzle surrounds the core of the framework, which is the engagement of patients and families.
This framework describes two main components of a healthcare system: the institutional culture and its learning system, with leaders connecting the two. An effective safety culture results from the interplay of psychological safety, fair, equitable, transparent and consistent accountability, team communication, and skillful negotiation that together create a positive workplace environment.
The learning system is the mechanism that allows the care team to thrive and continuously improve. It deliberately promotes continuous learning, transparently measures improvement efforts, and implements reliable processes. 4
At the core of the framework is the engagement of patients and families. The goal of all quality improvement efforts is the safety of patients across the continuum of their care. Frankel et al 4 acknowledge that both culture and learning are intimately interconnected.
Collapse section
Leadership is integral to the establishment and maintenance of both the learning system and institutional culture.
Leaders at all levels set the stage for the successful integration of the safety culture and the learning system. Generally, they have four main responsibilities:
- Protecting the values of the organization by designing reliable systems and by appropriately responding to provider behavioural choices.
- Fostering trust and respect, valuing provider opinions, effectively dealing with abusive or unprofessional behaviour.
- Creating psychological safety, and encouraging and listening to the opinions of providers, patients, and families.
- Promoting learning by understanding and applying improvement science, reliability science, and continuous quality improvement; and by inspiring that work throughout the organization.
Leaders can demonstrate their own engagement by doing regular executive walkarounds. Through these rounds, leaders gain opportunities to converse with frontline providers and get feedback about their past decisions. Because feedback without action adversely affects the learning system and leads to low engagement, skilled leaders listen intently, act on the feedback, and make corrective actions visible.
Healthcare leaders can strive to promote a shared mindset and application of practices in support of all elements of the framework.
Psychological safety
Psychological safety is the solid foundation needed to support a learning system and a positive workplace culture. 5 In teams that provide highly reliable outcomes, all individuals—from housekeeping staff to the chief physician—feel safe to ask questions without fear of appearing to lack knowledge, to ask for feedback without fear of being perceived as incompetent, to be respectfully critical of a plan without being labeled as disruptive, and to offer suggestions for improvement without being considered negative.
Everyone must create and support psychological safety as part of their job. To lay the groundwork for psychological safety, organizations need to clearly convey to all staff and leaders that it is an expectation.
Accountability
To be accountable is to be professionally responsible or answerable. Healthcare providers should be held accountable for their actions and not for system flaws or processes over which they have no control.
Every healthcare professional is accountable to:
- make behavioural choices that align with their institution/facility’s values promoting safe care
- maintain their knowledge and skills
- act professionally
- follow sound policies
- report system vulnerabilities
- be aware of and mitigate potential personal performance modifying factors (hunger, illness, etc.) that can impact their ability to practice safely
Through the policies they develop and through their application, leaders must convey to all providers that when faced with a complaint, providers will be made aware of its elements, have the opportunity to respond, and know that decisions will be unbiased and fair.
Teamwork and communication
Teams that provide highly reliable care communicate clearly and anticipate problems before they occur. Individual healthcare providers put their personal preferences aside, harmonizing their approach to care and communication, while demonstrating flexibility.
Teams can minimize limitations of individual cognition and mitigate for potential error by fostering a culture where anyone feels comfortable and responsible to “stop the line”—to interrupt a process of care—at any time if they perceive there is a risk to patient safety. Team members understand that mistakes are inevitable and openly invite others to respectfully challenge them in an effort to prevent harm. Even when team members who speak up are wrong, they are encouraged to speak up again.
Team briefings, debriefs and huddles help create situational awareness and help promote an understanding of what is happening at the moment and allow for the projection of that comprehension into the future to guide safe actions. Teams also use these activities as a way to identify issues for improvement, which serves as input to the learning system.
Negotiation
Healthcare is complex and healthcare providers must find ways to manage conflict and negotiate solutions while maintaining relationships. When resolving conflicts, they focus on interests (i.e. needs, fears, ambitions, goals) rather than positions or demands. They seek to repair and maintain relationships when making decisions on corrective actions. Psychological safety lays the foundation for successful negotiation.
Collapse section
Continuous learning
Healthcare organizations need to be committed to continuously finding ways to deliver safe, effective care. Continuous learning needs to include both the proactive and real-time identification and prevention of harm as well as the ability to learn from patient safety incidents (accidents in Québec).
The learning needs to be shared across the organization and across organizations. Time and resources need to be dedicated to learning what is working and what is not. Feedback must be given to providers who report patient safety incidents or potential failures, so they know every report is reviewed and appropriately actioned, thus fostering ongoing engagement in reporting.
Learning boards (or huddle boards) are tools that facilitate proactive learning from locally identified quality improvement projects. Learning boards are visual boards used by local teams during learning huddles to address locally identified risks and the progress of the process for improvement. 6 Through their constant visibility, they also serve as daily reminders of the importance of quality improvement work to the culture of the unit. The use of learning boards can improve team engagement, and learning for team members, who come to see themselves as allies for improvement. By meeting regularly, the team engages in quality improvement and continuous learning using improvement metrics that are important and relevant to them.
To be most effective, team huddles need to foster psychological safety to allow for maximum participation and learning.
Improvement and measurement
This component of the framework refers to leveraging quality improvement science to develop, test, implement, and spread improvement efforts across the organization.
To achieve highly reliable outcomes, teams use feedback and rapid PDSA (Plan, Do, Study, Act) cycles to objectively measure the impact of their improvement efforts. Team leaders empower and enable frontline providers to take ownership of improvement and support them in learning to recognize potential problems, identify and try solutions, and measure the solutions’ impact. While many institutions have developed outcome measures, effective teams supplement these with clinically meaningful process measures to gauge the impact of their quality improvement efforts. These measures are then posted to the team learning board as a visual demonstration of the real-time results of improvement efforts that can be used to adjust subsequent iterations of the PDSA cycle.
Reliability
While quality healthcare is about how well health services are delivered, reliability is concerned with how consistently quality services are delivered day after day, in real-world circumstances. The goal is to provide the appropriate care, to the right patient at the right moment, every time. The challenge for healthcare is the complexity of the systems of care and human fallibility. The focus needs to be on how the work is done, not on who does it.
At the population level, reliability leads to improved outcomes. The best care becomes the usual care.
- Necessary variation can promote safe care by accounting for a patient’s special needs and modifying the process of care to meet them.
- Unnecessary variation based on individual provider choices can lead to harm by introducing unusual steps or procedures that may lead to confusion among the healthcare team.
The science of reliability involves four key steps to reduce variation:
- Standardize: doing the same things in the same way every time.
- Simplify: making processes as simple as possible to decrease the opportunity for mistakes.
- Reduce autonomy: care delivery follow evidence-based best practices (as opposed to personal preferences) unless change is required to meet a specific patient’s needs.
- Highlight deviations from practice: when it is in their patient’s best interests, providers sometimes deviate from standard policies and procedures. The deviation should be documented so it can be analyzed. Sometimes it becomes necessary to correct the system factors contributing to the drift from the standard practice. However, the noted deviation may sometimes indicate that a more efficient process has been developed on the front lines and that an adjustment to the current policy is required to reflect the improved practice.
Reliability must be monitored and measured. Patients benefit from a higher quality of care and providers benefit from decreased cognitive load. Psychological safety and team cross monitoring encourage speaking up when drift away from standard practice is occurring. Within a culture of accountability, it is generally recognized that behavioural drift is the single greatest threat to patient safety, owing to its unconscious nature and to its pervasiveness in everyday practice.
Transparency
Transparent organizations make it clear how decisions are made, and how improvement is tracked such that patients and their families, staff, physicians, and leaders can see the learning system in action. Transparency means displaying openness, accountability, and clear communication of values and expectations.
Transparency among clinicians exists when there is no fear of giving suggestions, pointing out problems, or providing feedback.
Transparency with patients, specifically after a patient safety incident (accident in Québec), involves communicating directly and disclosing what has occurred and explaining what system changes have been implemented to prevent the event from happening again.
Transparency among organizations includes sharing good practices and the lessons learned, as well as about improvements made to systems as the result of incident reviews.
Collapse section
The concept behind Safety-I is the investigation of patient safety incidents (accidents in Québec) looking for quality improvements that will decrease the risk of the event reoccurring. It is a “find the cause and effect” exercise. It seeks to improve the safety of care by focusing on what goes wrong. Safety-I’s foundation is based on two concepts:
- The system can be decomposed into its component parts.
- There are only two possible modes of operation: things went correctly or things went wrong. 7
As medical advances and healthcare delivery is increasingly complex, providers must be flexible, adaptive, and able to adjust to the unexpected. They do this very well.
The Safety-II premise is that instead of only looking at the few cases where things go wrong, we should also consider the many cases where things go well. To understand why things go right, we need to look at the everyday functioning of the system.
Safety-I and Safety-II are complimentary activities. Whereas Safety-I is reactive when things go wrong, Safety-II is proactive, continuously looking at what is going right, but could go wrong.
Collapse section